October 25, 2024 - By Laura López González - Colorectal cancer cases are rising among younger people, striking even folks without obvious risk factors.
For nearly two decades, UC San Francisco Family Community Medicine Professor Micheal Potter, MD, has worked to make cancer screening easier.
But getting otherwise healthy adults in for regular tests to detect cancer early is more complicated than it seems. More than 15 years ago, Potter worked with San Francisco community health clinics to develop a model that paired colorectal cancer screening with something about half of us do annually anyway: get a flu shot.
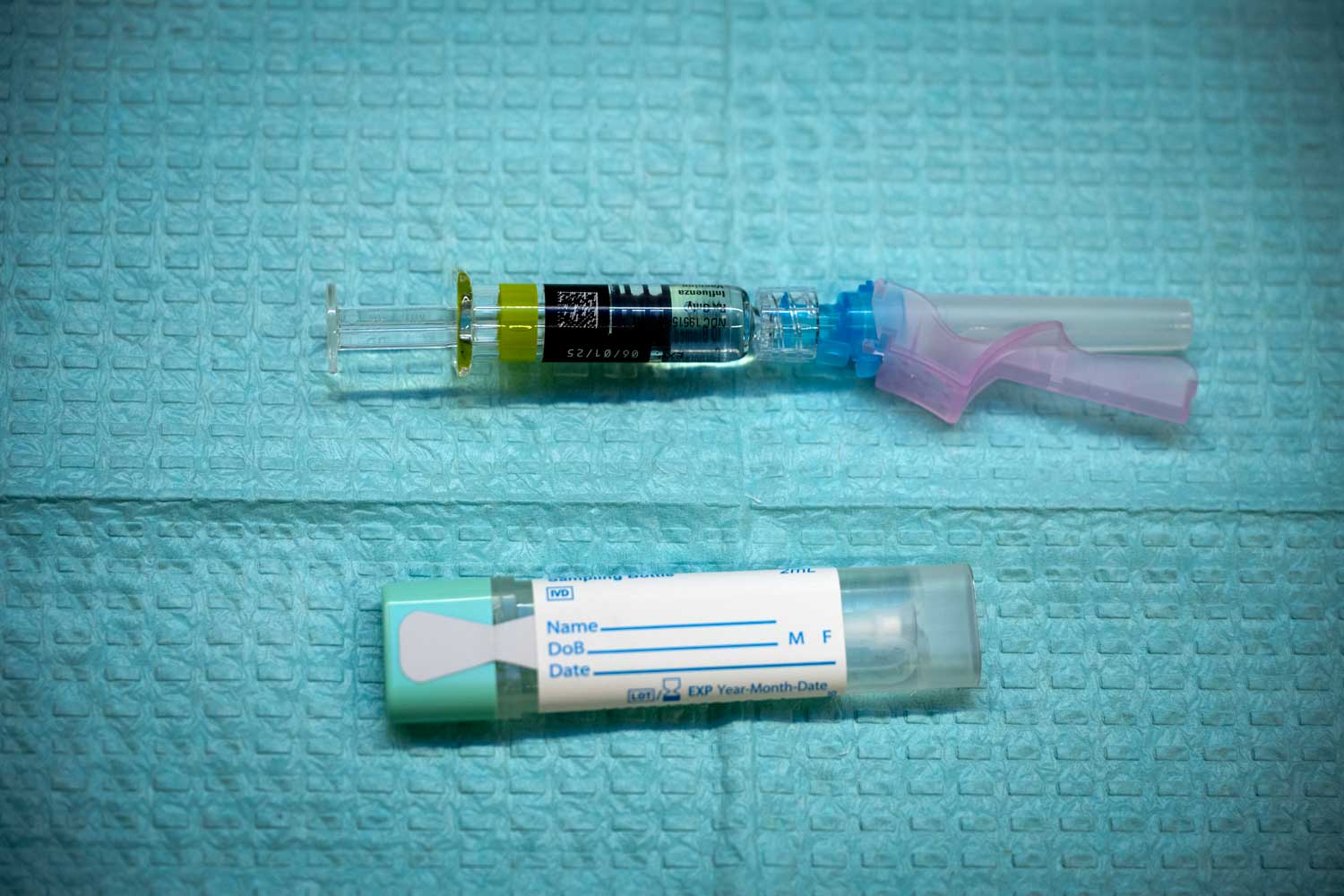
The model has community clinicians offer take-home fecal immunochemical tests (FIT) for colorectal cancer alongside flu shots in a model dubbed FluFIT. Folks who opt for the screeners can collect samples at home before sending them to a lab for tests.
Today, community health centers in all 50 states have used Potter’s model, first developed at UCSF to save lives. Potter tells us how colorectal cancer risk is changing and what to know about screening.
How has colorectal cancer risk changed?
The risk of colorectal cancer increases with age, and the vast majority of people who get colorectal cancer are above 50. But over the last few years, we’ve seen that people who are in their 40s develop about the same risk of colorectal cancer as people in their 50s would have had two decades ago.
Why are people getting colorectal cancer at younger ages?
We don’t yet know why people are developing cancers earlier, but this seems to be a global phenomenon and not just restricted to colorectal cancer. A lack of physical activity, increasing rates of obesity or toxic substances in our food supply, such as microplastics, could be why we’re seeing more cancer in younger people.
When should I start screening for colorectal cancer?
Because of the shift toward younger people being diagnosed with colorectal cancer, most U.S. guidelines now recommend screening beginning at age 45 instead of waiting until age 50, as was previously recommended.
Doing a FIT every year is enough. For most people, it’s equivalent to getting a colonoscopy once every 10 years.
Does this change if I have a history of colorectal cancer in my family?
Yes. People with known risks for colorectal cancer, such as a parent or sibling diagnosed with colorectal cancer at a young age, or with multiple family members diagnosed with it, should be screened earlier. People with a family history of colorectal cancer should make sure their doctor is aware. For those with familial genetic disorders that predispose to colorectal cancer, screening before age 45 can be very important.
How does FIT work?
This test detects microscopic amounts of human blood protein in the stool, which is a sign of bleeding that could be coming from early cancer or from a polyp that could develop into cancer if left untreated.
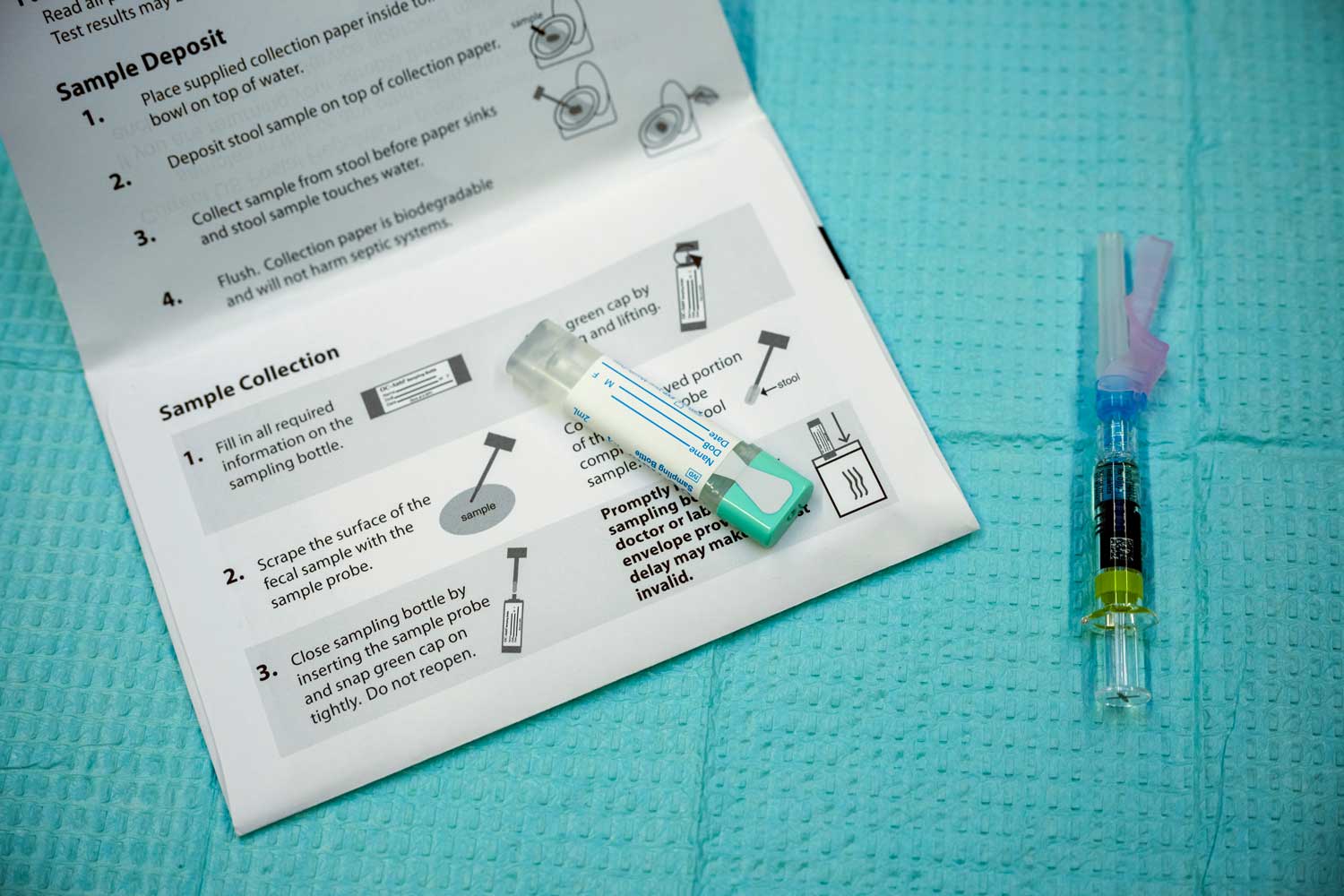 A fecal immunochemical test (FIT) seen here with a flu shot. Patients can request these take-home screeners during their flu vaccination, or from their clinics. Photo by Deanne Fitzmaurice
A fecal immunochemical test (FIT) seen here with a flu shot. Patients can request these take-home screeners during their flu vaccination, or from their clinics. Photo by Deanne FitzmauriceHow often should I get a FIT?
While colon polyps and cancers usually develop slowly over many years, lesions can be missed if you only get the test sporadically. However, in terms of saving lives, doing a FIT every year is enough. For most people, it’s equivalent to getting a colonoscopy once every 10 years.
What happens if I test positive?
If the FIT results are abnormal, this should be followed up with a colonoscopy, which is an examination of the entire colon performed by a gastroenterologist. A colonoscopy is a 30-minute procedure done under sedation and is painless. It requires taking laxatives to clean out the bowel and a day off work to do the procedure and recover.
If my FIT test is abnormal, how quickly should I schedule a follow-up with my doctor?
I cannot emphasize enough how important it is to get a timely colonoscopy after an abnormal FIT. Ideally, the colonoscopy should take place within three months of the abnormal FIT result. Failure to follow up promptly can lead to delays in diagnosis that can have catastrophic consequences for patients.
My clinic doesn’t offer colorectal cancer tests during flu vaccinations. How else can I get a take-home test?
Most clinics will provide these tests during routine primary care visits. If you think you are due for screening, call your clinic, and they can probably mail you a kit.
How does a FIT test compare to the new, recently approved blood tests for colorectal cancer?
Although it may seem more convenient to get a blood test than to get a stool test, the new blood tests have some drawbacks. They remain expensive by comparison. In addition, while they are very good at detecting advanced cancers, they are not so good at finding polyps or early-stage cancers that we really want to know about to save lives. For now, in my view, stool tests are superior to the newer blood tests in terms of cost and their ability to save lives.
I’m younger than 45, does that mean I’m not at risk for colorectal cancer?
Not necessarily. People in their 30s and 40s with persistent changes in bowel habits or rectal bleeding should make sure to consult their doctors and ask specifically about whether their symptoms could be caused by colorectal cancer.
Although these symptoms, after full evaluation, usually prove to be something else (like irritable bowel syndrome or hemorrhoids), care should be taken to rule out more serious causes, such as colorectal cancer, ulcerative colitis or Crohn’s disease.
One of the reasons why people in their 30s and 40s who develop colorectal cancer have worse outcomes than people who are diagnosed at older ages is that their symptoms are not taken seriously or evaluated until the cancer is already very advanced.
Source: UCSF

