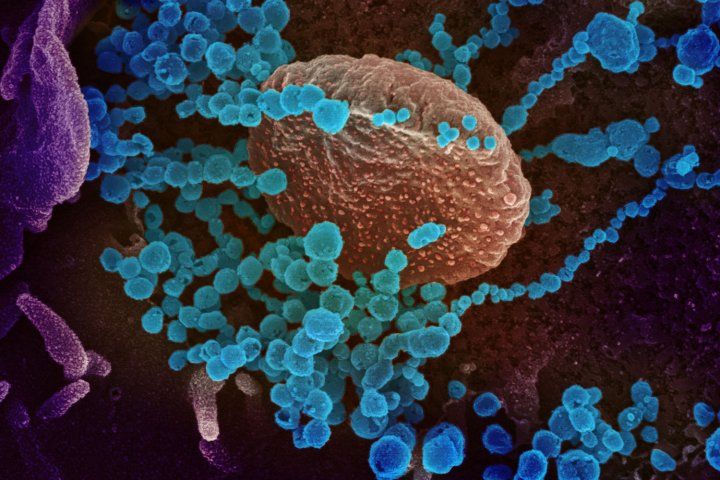
Scanning electron microscope image of the new coronavirus, SARS-CoV-2 (blue), emerging from the surface of cells cultured in the lab. Image credit: NIAID-RML
WHAT IS THE NOVEL CORONAVIRUS?
-
The novel coronavirus, also known as SARS-CoV-2, was identified as the cause of an outbreak of respiratory illness first detected in Wuhan, Hubei Province, China.
- COVID-19, the disease caused by the new coronavirus, has since been identified in most of China as well as in dozens of countries on six continents.
- Coronavirus refers to a family of viruses that cause a spectrum of diseases ranging from the common cold to severe life-threatening pneumonia.
- They’re named for the spike proteins on the surface of the virus that make the virus look like a crown or star.
- There are seven coronaviruses known to infect humans.
- The emergence of two of these coronaviruses, SARS in 2002 and MERS in 2012, occurred as a result of animal-to-human, or zoonotic, transmission events. The same is likely true for the new coronavirus.
March 2, 2020 - By Nina Bai - As COVID-19, the disease caused by the novel coronavirus, continues to spread around the world, the U.S. Centers for Disease Control and Prevention has advised organizations to prepare for possible community transmission in the United States.
As concerns about the outbreak begin hitting closer to home, UC San Francisco infectious disease experts are providing the latest updates on what the public needs to know.
Deborah Yokoe, MD, MPH, medical director for hospital epidemiology and infection prevention at UCSF Health, and Robert Kosnik, MD, director of the UCSF Occupational Health Services, addressed some common concerns about the new coronavirus.
How do I protect myself and my family against the new coronavirus?
“The best way to protect yourself and your family from COVID-19 is to follow all the same basic practices that are important for protecting yourselves from influenza,” said Yokoe.
According to the U.S. Centers for Disease Control and Prevention (CDC), these include
- Washing hands often with soap and water for at least 20 seconds
- If soap and water are not available, using an alcohol-based hand sanitizer with at least 60 percent alcohol
- Avoiding close contact with people who are sick
- Avoiding touching your eyes, nose, and mouth
- Covering your cough or sneeze with a tissue, then throwing the tissue in the trash, and washing your hands
- Cleaning and disinfecting frequently touched objects and surfaces
- Staying home when you are sick
Should I start wearing a mask when I’m at work or out in public? If not now, when might that change?
The CDC and other public health experts do not recommend that people who are well wear face masks as a way to protect themselves from respiratory illnesses, including COVID-19.
As there is currently a limited global supply of masks, they should be reserved for caregivers of patients with infections that require mask use or by patients with cough or other symptoms of respiratory illness.
“In hospitals like the UCSF Medical Center,” said Yokoe, “we do ask patients who are sick with respiratory illnesses to wear a mask as a way to contain the respiratory droplets that are produced when they cough or sneeze in order to prevent spreading infections to others.”
Kosnik explained that masks are more effective when worn by someone who is sick to prevent respiratory droplets from escaping – so if you are sick, it may be a public service to wear a mask if you need to be out and about.
“If there were widespread community transmission, like the kind in some parts of China, then there may be some advantage to wearing a mask out in public – but we’re a long ways away from that here,” said Kosnik.
What are the symptoms of COVID-19? Is it possible to distinguish from a cold or flu?
The symptoms of COVID-19 infections can range from very mild to severe respiratory illness and may include fever, cough and shortness of breath. These symptoms can be very similar to those for influenza, so it may be difficult to distinguish without clinical testing.
“We are still learning more about COVID-19 every day,” said Yokoe, “But based on the most comprehensive information that we have so far from China, about 80 percent of COVID-19 infections were thought to be mild infections and a small proportion of people developed severe pneumonia.”
When should I seek medical attention if I’m worried about the coronavirus? What’s the best way to do that?
If you have not traveled to an area of the world with sustained community transmission of COVID-19 within 14 days of feeling sick, you should follow the same steps that you would take if you thought you had the flu. These include staying home from work or school, unless you feel that you need medical attention.
If you have traveled to infected areas, or had contact with someone who has, and feel sick with a fever, cough, or difficulty breathing within 14 days, you should call your doctor’s office, urgent care clinic, or emergency department ahead of time and tell them your recent travel and symptoms. They can help to make decisions about whether, when and where you be evaluated.
Currently, nearly all the people in the U.S. with confirmed COVID-19 infection were exposed through travel to a country with widespread transmission or close contact with someone who had – although this may change over time.
If I don’t have health insurance, can I still get care?
“Anyone who requires medical care can receive care, regardless of insurance status,” said Yokoe.
What are the testing criteria for COVID-19 now that there is a suspected case of community transmission with no travel history?
Decisions about testing currently are made on a case-by-case basis by the CDC in discussion with health care providers, infection prevention experts, and public health departments. “The CDC testing criteria for COVID-19 have just recently been updated and will likely continue to change as the situation continues to evolve,” said Yokoe.
The CDC’s persons under investigations (PUI) criteria, which offer guidance on who to test for COVID-19, were updated after the first suspected case of community transmission was reported in the U.S. The current criteria include
- Fever or symptoms of respiratory illness (e.g., cough or shortness of breath) in someone who’s had close contact with another person with a positive COVID-19 test result.
- Fever and symptoms of respiratory illness severe enough to require hospitalization in someone who traveled to a country with widespread or sustained community transmission of COVID-19.
- Fever and severe pneumonia requiring hospitalization without an alternative explanatory diagnosis (such as the flu).
Currently, most testing is still done at the CDC, but Yokoe said there is ongoing work to increase the capacity for testing on the state and local level, as well as research to develop new rapid diagnostics.
CORONAVIRUS Q&A
Infectious disease expert, Charles Chiu, MD, PhD, explains how the COVID-19 spreads and progresses. Read more
How are hospitals preparing for COVID-19?
Hospitals, including UCSF Medical Center, are working hard to prepare for the possibility that COVID-19 could spread within the U.S., which includes creating plans for outpatient clinics, emergency departments, and inpatient settings so they are flexible enough to care for larger numbers of patients with COVID-19.
“At UCSF Health, we have activated our emergency command centers and are meeting several times daily to stay on top of the situation,” said Yokoe. “We are working closely with the San Francisco, Alameda County, and California Departments of Public; the CDC; and other area hospitals.”
“We are ensuring that all CDC recommendations for caring for patients with COVID-19 are in place, such as being able to put these patients into the right type of hospital rooms, making sure that appropriate personal protective equipment (such as respiratory protection, gowns, and gloves) are available, and that staff who will be caring for these patients are able to use that equipment correctly.”
San Francisco Mayor London Breed declared a public health emergency on Feb. 25, 2020, to enable the city to mobilize resources, accelerate emergency planning, streamline staffing, coordinate agencies and allow for future reimbursement by state and federal agencies, if the need arises.
If UCSF Health is treating COVID-19 patients, will other patients be safe in the hospital?
UCSF Health cares for patients with some of the most complex health conditions and is highly experienced in infection prevention and control. Its infection prevention practices and protocols are aimed at ensuring that faculty, employees and contractors, as well as other patients and visitors remain safe in the hospital.
UCSF Health has put into the place CDC-recommended infection prevention protocols and procedures to prevent spread of infection from patients with COVID-19, said Yokoe.
These include placing patients with confirmed or possible COVID-19 infection into isolation rooms with negative pressure and special ventilation to prevent the spread of illness to other patients and staff. UCSF Health has over 40 airborne infection isolation rooms and can adapt additional rooms to care for larger number of patients, if needed.
Source: UCSF








